Developmental Screening Step 2: Train
Training the team occurs in two parts.
Part 1 focuses on how to use the recommended screening tools for each domain. A summary of each recommended tool is presented below.
Part 2 focuses on conversations with families. This includes the importance of reviewing results with families and navigating conversations when a screen indicates “monitoring” is needed or when a screen results in “at risk”.
Training Part 1: Screening Instruments
Staff members who are involved in developmental screening require instruction on how to introduce, administer, and score each screen (unless they are using a tool that automatically scores such as the Well- Visit Planner).
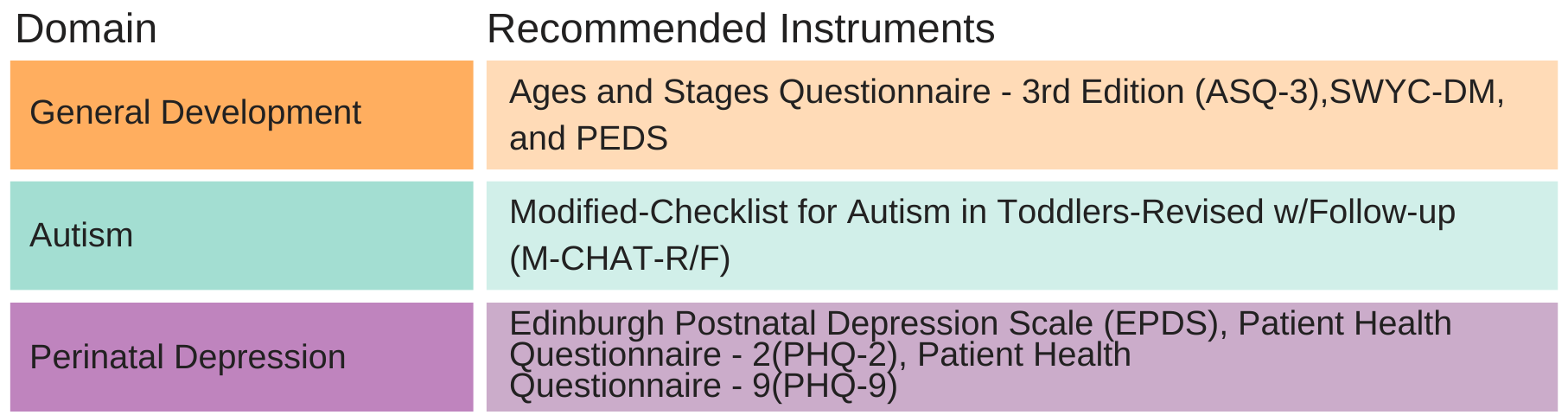
Developmental Screening for General Development—Featured Tools
Recommended Tool: Survey of Well-being of Young Children – Developmental Milestones Survey (SWYC-DM)
The Survey of Well-Being of Young Children-Development Milestones (SWYC-DM) is a validated developmental screening tool that helps identify children at risk for developmental, behavioral, and social delays.
- Cost: There is no cost to use paper/pencil surveys or use online as a part of the Well Visit Planner and access automated results on the provider data dashboard. There is an option to pull results/findings into the Electronic Health Record. SWYC is included in EPIC for providers using this system.
- Languages Available: Arabic, Bengali, Burmese, Chinese, Chuuksee, English, French, Haitian-Creole, Khmer, Korean, Nepali, Portuguese, Russian, Samoan, Somali, Spanish, Tagalog, Traditional Chinese, Vietnamese (English and Spanish only if used as part of the Well Visit Planner)
- Age Range:1 month – 5 years and 6 months
- What is Assessed: Communication, fine motor, gross motor, personal-social, problem solving
- Length: 10 questions
- Time to Complete: 1 minute or less
- Time to Score: Automatic if using the Well Visit Planner; 1.5 minutes if by hand. Additional time if you scan findings into the Electronic Health Record
- When to screen: 9, 18, and 30 month well-child visits (other ages available for surveillance or when concern is present)
- For further information and instruction on the SWYC-DM and tools click here. For more information about the Well Visit Planner, which includes the SWYC, click here.
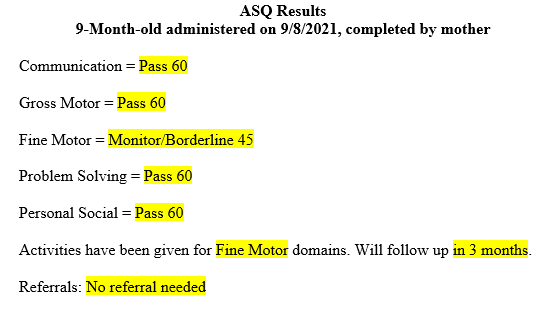
Recommended Tool: Ages and Stages Questionnaires, Third Edition ((ASQ®-3)
The Ages and Stages Questionnaires-3rd Edition is a validated developmental screening tool that helps identify children at risk for developmental, behavioral, and social delays.
- Cost: $295 for starter kit with paper/pencil surveys. Three options, each with an additional fee are available: (1) an online electronic system (Pro or Enterprise) to allow providers to enter family data and receive automated scores ($500); (2) an online family completion platform (ASQ Online) used with the Pro or Enterprise ($350); and (3) an option to have ASQ scores pulled into the Electronic Health Record (varies; $800 for 1000-2000 screens).
- Languages Available: Arabic, Chinese, English, French, Spanish, Vietnamese
- Age Range:1 month – 5 years and 6 months
- What is Assessed: Behavior, communication, fine motor, gross motor, personal-social, problem solving
- Length: 30 questions
- Time to Complete: 10 – 15 minutes
- Time to Score:1-3 minutes (online option to enter data and generate an automatic score) Additional time for completion of paper version scoring and then scanning into the chart dependent upon clinic process
- When to screen: 9, 18, and 30 month well-child visits (available for other ages for surveillance or when concern is presented)
- For further information and instruction on the ASQ and tools click here.
Recommended Tool: Parents’ Evaluation of Developmental Status (PEDS)
The Parents’ Evaluation of Developmental Status (PEDS) is a validated developmental screening tool that helps identify children at risk for developmental, behavioral, and social delays.
- Cost: $349 for starter kit, options for online data entry and scoring and to transfer the scored instrument into the Electronic Health Record for additional fee.
- Languages Available: Print available in English and Spanish. Can be licensed in 60+ languages.
- Age Range: Birth – 8 years
- What is Assessed: Behavior, communication, fine motor, gross motor, personal-social
- Length: 10 questions
- Time to Complete: 5 minutes
- Time to Score:2 minutes. Option for online scoring for additional fee. Additional time for completion of paper version scoring and then scanning into the Electronic Health Record.
- When to screen: 9, 18 and 30 month well-child visits (other ages available for surveillance or when concern is present)
- For further information and instruction on the PEDS and tools click here.
Developmental Screening for Autism—Featured Tool
Recommended Tool: Modified Checklist for Autism in Toddlers Revised (M-CHAT-R/F)
Symptoms of Autism Spectrum Disorder (ASD) often become apparent during the child’s first year and can be identified by 18 months. This screen has two stages if a concern is identified. First, a 20-item questionnaire helps identify children at risk for ASD. The second stage, a short follow-up interview completed with the family immediately after the initial screen occurs if a concern is indicated and reduces the number of false positive results.
- Cost: There is no cost. It is also included as part of the Well Visit Planner.
- Languages Available: 40+ languages. Available in English and Spanish if used via Well Visit Planner
- Age Range:16 – 30 months
- What is Assessed: Risk for Autism Spectrum Disorder
- Time to Complete: 5-10 minutes for initial questionnaire
- Time to Score: Initial score 1 minute, additional 10 minutes if follow-up interview is necessary (i.e., if initial score is between 3-7). Automatic scoring and reporting if use Well Visit Planner. Can be scanned into the Electronic Health Record.
- When to screen: 18 and 24 month well-child visits
- For further information and instruction on the M-CHAT-R/F™ and tools click here. For more information about the Well Visit Planner click here.
Screening for Perinatal and Postpartum Depression—Featured Tools
Recommended Tool: Edinburgh Postnatal Depression Scale (EPDS)
The EPDS was developed to identify women who may have postpartum depression. Preferred tool for postpartum depression screening.
- Cost: No cost. Also included as part of the Well Visit Planner.
- Languages Available: English, Spanish
- Age Range: Not age dependent
- What is Assessed: Frequency of depressed mood and anhedonia over the past seven days
- Time to Complete: 5 minutes
- Time to Score: 2 minutes. Automatic scoring when used as part of the Well Visit Planner
- When to screen: 1, 2, 4, and 6 month well-child visits
Recommended Tool: Patient Health Questionnaire-2 (PHQ-2)
The EPDS was developed to identify women who may have postpartum depression. Preferred tool for postpartum depression screening.
- Cost: No cost. Also included as part of the Well Visit Planner.
- Languages Available: English, Spanish
- Age Range: Not age dependent
- What is Assessed: Frequency of depressed mood and anhedonia over the past two weeks
- Time to Complete: Less than 2 minutes
- Time to Score: Less than 1 minute
- When to screen: 1, 2, 4, and 6 month well-child visits
Recommended Tool: Patient Health Questionnaire-9 (PHQ-9)
In addition to recommending the Patient Health Questionnaire-9 as an option for initial screening for Perinatal Depression, we also recommend using it as a follow-up to a positive PHQ-2.
- Cost: No cost
- Languages Available: English, Spanish
- Age Range: Not age dependent
- What is Assessed: Frequency of depression symptoms over the past two weeks
- Time to Complete: Less than 2 minutes
- Time to Score: Less than 1 minute
- When to screen: 1, 2, 4, and 6 month well-child visits
All maternal depression screening tools can be integrated into the EHR.
NOTE: The Well Visit Planner also includes a post-partum depression screening tool using the Edinburgh Postnatal Depression Scale.
Online Platforms for Developmental Screening Tools
For those considering an electronic/online format, a comparison was made of the following online platforms.
Comparison of Key Features and Costs for Online Screening Tools
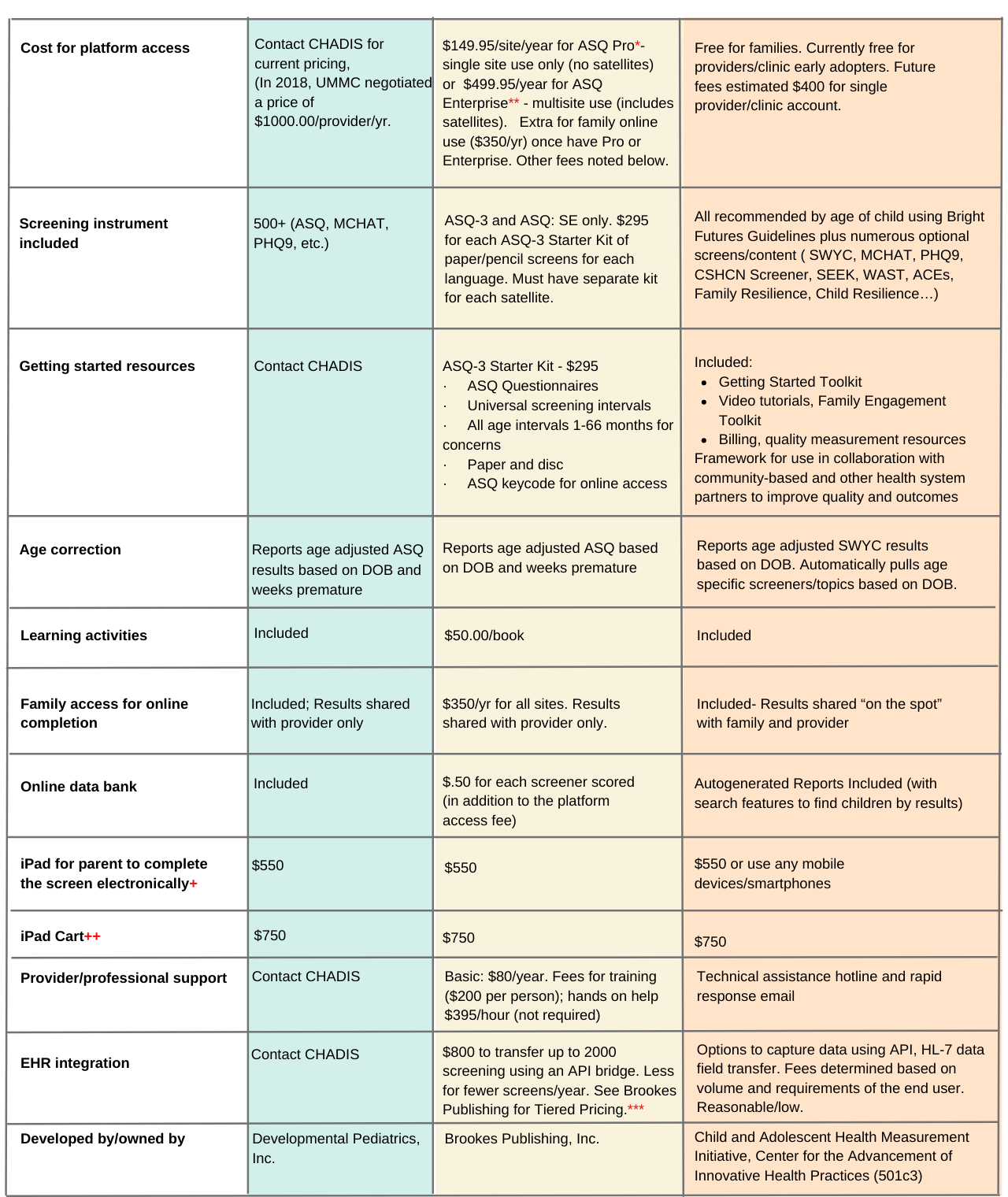
***See Brookes Publishing for Tiered Pricing
+iPad used so that patients did not share computer with access to a patient’s records
++iPad mounted on cart to eliminate likelihood that iPad would be removed from clinic, similar to computer on wheels
Note: For those choosing to perform paper screening, the ASQ-3 kit can be purchased without the addition of the online platform.
Please visit the AAP STAR Center Screening Tool Finder for more information on screening tools for use in the Pediatric Medical Home.
Documenting Results in the Electronic Health Record (EHR)
Integrating developmental screens and results into your practice’s electronic health record (EHR) helps ensure consistent service delivery and simplifies data tracking. All recommended screens can be scanned into the EHR. Alternatively, clinics can opt to have these automatically placed into the record using each tool’s API/HL-7 data transfer abilities. However, this option will require your EHR vendor/team to enable this to occur.
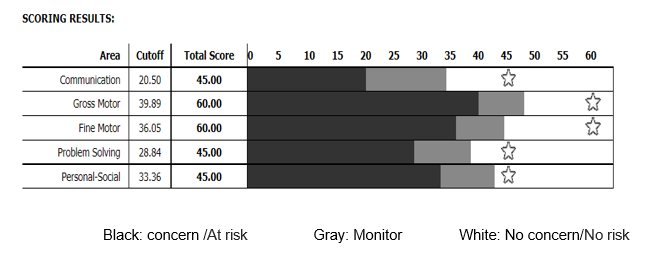
Option 1: When using an online platform, the medical staff may “copy and paste” the results by importing the performance chart from the online database into the patient visit note of the electronic record (see example below).
Option 2: Screening results can be entered into the EHR using a “dot phrase” (a dot followed by a short user-generated phrase which allows text to be easily inserted into patient notes) to document results. After generating the dot phrase, the provider adds patient scores to document screening results. It is possible to utilize this option whether the screening is completed on paper or electronically (see example below).
Billing and Coding
To maximize compensation, a clear understanding of billing processes related to developmental screening is necessary. It is important to ensure appropriate CPT codes and any modifiers are included in documenting screening procedures.
Developmental screening services are typically reimbursed but coverage varies depending on state and type of insurance provider. Children who are enrolled in Medicaid are entitled to all developmental screens recommended by AAP Bright Futures. These services are covered under the Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit. Children’s Medicaid also covers most of the interventions or services that are recommended after a screening. These services may include speech, occupational or physical therapies, and behavioral health services. Increasingly, private insurance carriers are improving coverage for screening and recommended services.
Increasingly, insurance carriers are reimbursing developmental screening. Typically, carriers reimburse for the three universal developmental screening visits and the two recommended screening visits for autism. You can advocate for payment reform through your organization’s legislative liaison or your local AAP.
EPSDT Billing/Coding
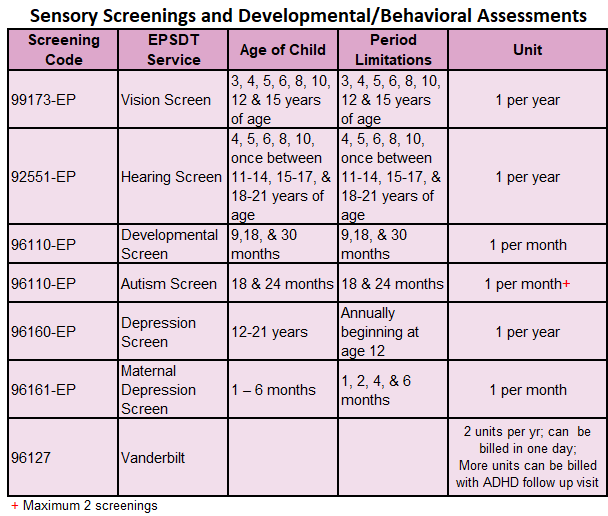
If there is a concern on a developmental or autism screen, the provider must document in the medical record the screening tool(s) used, the result of the screen, and any action taken.
Since both developmental screening and MCHAT are recommended at the 18 month visit and are billed under the same procedure code (96110) for the same day of service, some Medicaid Managed Care groups, as well as some insurance carriers, have difficulty recognizing both should be reimbursed. Providers may only receive reimbursement for one developmental and one autism screen per day of service.
To receive reimbursement for both services performed on the same day, providers may submit claims for two units of the relevant procedure code. If a child is at-risk or suspected of a developmental abnormality, developmental and autism screenings qualify as a covered service, when administered at intervals outside of EPSDT preventive visits.
Perinatal Depression Screen: To bill for depression screening documentation must include the tool used, the results, and any follow-up actions taken. If an enrollee’s caregiver screens positive, the provider must refer the caregiver to available resources, such as their primary care provider, obstetrician, or mental health professionals, and document the referral.
Training Part 2: Conversations with Families
Once a screening is completed, it is important to discuss the results with the family and offer next steps as needed. Even if results are negative, anticipatory guidance for families in terms of growth and development of their children across all domains, should be part of every wellness visit. Developmental discussions and concerns should be family centered.
Conversations with families should emphasize realistic timelines for achieving developmental milestones and should be culturally sensitive to each family. Using milestone checklists, such as those provided by the CDC’s Learn the Signs. Act Early, can help guide the conversation and serve as a helpful take-home tool for families. This resource may also be helpful: Development is a Journey – Brazelton Touchpoints. If using the Well Visit Planner, family resource sheets are provided based on results from the SWYC to support conversations. A Personalized Connected Encounter approach to visits is also provided. More resources are located on the Mississippi Thrive Resources page.
Screening Results: No Risk
Even when results show no concerns, it is still important to review results with the family and offer anticipatory guidance.
Screening Results: Monitoring
When a screen indicates a borderline performance in one or more domains, the following should occur:
- Close monitoring and follow-up,
- Offer developmental promotion activities, such as the ASQ Learning Activities, which help enhance skills in the area of concern,
- Re-evaluation in 1-3 months
– According to AAP guidelines, if the child remains in the monitoring range, or falls to the “at risk” range on follow up, referral for further evaluation should occur.
Screening Results: At Risk
When a child falls in the “at risk” range, further assessment is required. It is crucial to discuss findings and involve family in decision-making. All children under 3 years of age with developmental concerns should be referred to Early Intervention (Part C) for further evaluation and treatment. Children over 3, should be referred to Child Find (Part B), which is part of the public education school system.
Important points to emphasize about Developmental/Behavioral Screening:
- A screen that indicates risk is not a diagnosis, but it indicates that further evaluation is needed to determine necessary intervention.
- Early identification of developmental delays through appropriate screening increases timely referral to services and ultimately can improve both child developmental and behavioral outcomes.
Postpartum and Perinatal Depression Screen
Select from the following validated screening tools:
- Edinburgh Postnatal Depression Scale (EPDS)
- Patient Health Questionnaire 9 (PHQ-9)
- Patient Health Questionnaire 2 (PHQ-2) and, if positive, a full PHQ-9
Documentation must include the tool used, the results, and any follow-up actions taken. If a caregiver screens positive, the provider must refer the caregiver to available resources, such as their primary care provider, obstetrician, or mental health professionals, and document the referral.
About This Resource
The overarching goal of the Child Health and Development Project (Mississippi Thrive!) has been to improve developmental health outcomes for young children through the building of a statewide developmental and behavioral health system. As part of the system build MST worked with health care providers to increase developmental screenings, connect more children to the services they need, and equip providers with materials and resources to promote developmental and behavioral health with caregivers at wellness visits. Additional work was conducted to advance more comprehensive, family-engaged, whole child approaches.
This toolkit provides information about the specific resources and approaches used to support health care providers at the University of Mississippi Medical Center to integrate developmental screening and additional approaches to engage families and conduct comprehensive screening and personalized health promotion into their pediatric practices as well as lessons learned. It was modeled after the Louisiana Developmental Screening Toolkit created by the Developmental Screening Initiative at the Louisiana Bureau of Family Health. It incorporates a Continuous Quality Improvement framework based on the clinical practice guidelines form the American Academy of Pediatrics.
This toolkit was developed by the Mississippi Thrive! Enhanced Pediatric Medical Home Services (EPMHS) team in partnership with The Child and Adolescent Health Measurement Initiative (CAHMI). The Child Health and Development Project: Mississippi Thrive! (CHDP) was a project of the University of Mississippi Medical Center’s (UMMC) Center for the Advancement of Youth (CAY) and the Social Science Research Center (SSRC) of Mississippi State University (MSU).
This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling $17.4 million with 0 percent financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the U.S. Government. For more information, please visit HRSA.gov today. The Child and Adolescent Health Measurement Initiative (CAHMI) is a national non-profit initiative founded in 1996 to promote the early and lifelong health of children, youth and families using family-centered health and health care quality data and improvement tools and research. The Cycle of Engagement Well Visit Planner approach was developed and is maintained by the Child and Adolescent Health Measurement Initiative (CAHMI).